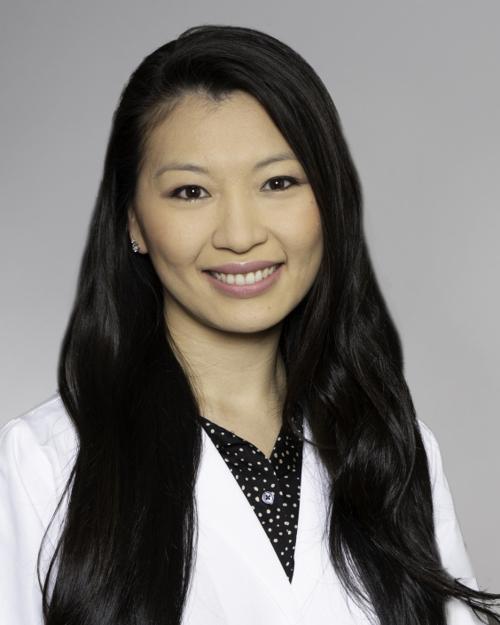
Nuvance Health Digestive Health Institute: Why choose us?
You’re in good hands at Nuvance Health, where teams include fellowship-trained gastroenterologists and experienced nurses. We regularly care for patients with disorders affecting the esophagus, stomach, small intestine, colon, rectum, gallbladder, pancreas and liver. Highlights of our program include:
-
Comprehensive care
We take time to get to know you as an individual, which helps us tailor recommendations. You have access to sophisticated options, including nonsurgical procedures and innovative therapies. Some offerings are only available in highly experienced programs, such as ours.
-
Convenience
Digestive health specialists are available in locations throughout New York’s Hudson Valley and Western Connecticut. And our coordinated approach makes it easier to receive the services that are right for you. We collaborate with other Nuvance Health specialists you are seeing to manage complex conditions.
-
Research
We participate in clinical trials evaluating new treatments, including inflammatory bowel disease (IBD) drugs. Patients who take part in these efforts get early access to new therapies and receive support from an experienced research team. Explore Nuvance Health Research and Innovation.
-
Leadership
Nuvance Health has been a destination for advanced medical education for decades. We host a 3-year Gastroenterology Fellowship Program that trains the next generation of digestive health specialists – an honor that is only awarded to programs like ours that see a high volume of patients and regularly treat complex cases.